In a world rife with inefficiencies, the healthcare sector grapples with the daunting challenge of accurate and timely diagnoses, particularly in complex cases like lung cancer. The traditional methods of diagnosis often require extensive data analysis, involving the painstaking task of reviewing previous medical records and imaging, a process that could take doctors invaluable minutes—time that artificial intelligence (AI) could dramatically reduce to mere moments. In this enlightening podcast episode of “AI and Healthcare,” host Nika Newton sits down with Pelot Tran, the CEO and founder of Pharm Health, a pioneering company dedicated to harnessing AI’s potential to transform patient care. Tran’s journey into healthcare technology is deeply personal; after experiencing the tragic loss of his uncle to late-stage lung cancer—detectable through advanced AI tools—he became persistent to solve the significant barriers to AI adoption in healthcare. Together, Newton and Tran explore the urgent need for AI integration that could empower providers and ultimately save lives, while acknowledging the long road ahead to realize this vision.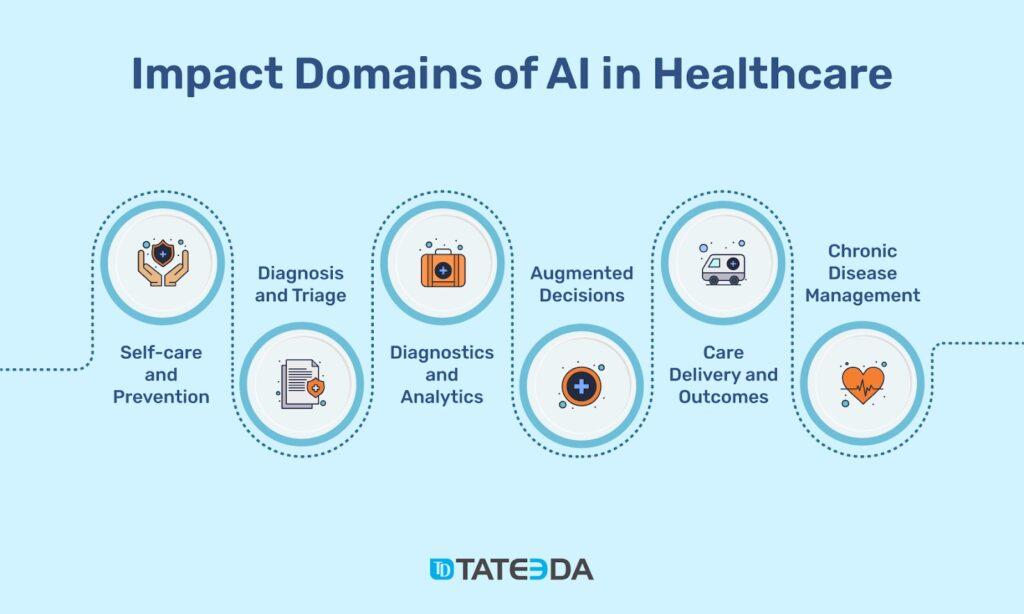
Challenges of AI Integration in Healthcare
The integration of AI into healthcare systems faces several obstacles that can hinder its potential benefits. First, there is a prevailing reluctance among healthcare professionals to adopt new technologies, often rooted in a fear of the unknown or concerns about the accuracy and reliability of AI-driven insights. This is compounded by the need for interoperability between AI tools and existing electronic health record (EHR) systems, which can lead to significant implementation challenges. Additionally, ethical considerations surrounding patient data privacy create a complex landscape, as stakeholders must navigate the regulatory frameworks governing data use and consent. This concern for data integrity not only impacts adoption rates but also raises questions about the validity of AI recommendations in clinical settings.
Moreover, the financial implications of incorporating AI technologies into healthcare practices cannot be overlooked. Organizations often face the daunting prospect of high initial costs associated with purchasing, implementing, and maintaining cutting-edge AI solutions. Smaller practices may find it particularly challenging to allocate resources for technology investments, leading to disparities in access to advanced care innovations. The workforce must also acquire new skills and training to effectively utilize AI tools, which can lead to additional educational burdens. As the industry works towards overcoming these hurdles, the collective push for improved collaboration among technology developers, healthcare providers, and regulatory bodies will be essential for fostering a smoother transition to AI-enhanced healthcare solutions.
The Human Element: Personal Stories Behind Technological Innovation
For many healthcare innovators,the journey into technology is often sparked by personal experiences that illuminate gaps in the system. Take the story of Dr.Sarah Lawson, a seasoned oncologist who faced the frustrating challenge of assisting patients battling cancer with limited resources. After losing her father to colon cancer,she harnessed her grief to develop an AI-driven tool aimed at flagging high-risk patients earlier.The emotional weight of her experience pushed her to envision a future where algorithms could analyze myriad patient data points quickly, leading to improved early intervention strategies and, ultimately, better patient outcomes. Her initiative reflects a growing trend: healthcare professionals are intertwining their lived experiences with innovations to enhance patient care.
Similarly, the story of Miguel Ramirez, a nurse, highlights the human aspect of tech integration. Frustrated by the inefficiencies in patient record access, he initiated a collaborative platform that uses AI to streamline dialog between medical staff and patients. His work not only improved workflow but also fostered a more compassionate approach to healthcare, where patient stories are prioritized alongside clinical data. This represents a broader movement within healthcare, where professionals strive for a balance between technology and the nurturing practice of medicine. As the sector evolves,these personal narratives drive the urgent need for tools that facilitate,rather than replace,the empathetic connections intrinsic to patient care.
Bridging the Gap: Strategies for Accelerating AI Adoption in Medical Practice
To effectively integrate AI into medical settings,it is crucial for healthcare organizations to foster a culture that embraces innovation and technology.Training and education programs tailored for healthcare professionals can enhance their understanding of AI capabilities and build trust in its applications. Moreover, establishing interdisciplinary collaboration among clinicians, data scientists, and technology developers can ensure that AI tools are optimized for clinical workflows. Engaging stakeholders throughout the implementation process not only addresses concerns but also promotes a sense of ownership and accountability among healthcare providers.
Additionally, addressing financial barriers is key to accelerating AI adoption. Organizations can explore partnerships with technology companies to share the costs and risks associated with AI implementation. Funding initiatives or grants focused on small practices can enhance equitable access to these technologies. Building a clear pathway for measuring the impact of AI on patient outcomes will also convince skeptics of its value, thereby leading to wider acceptance. By proactively identifying resources and support systems, the healthcare industry will be better positioned to navigate challenges and embrace the transformative potential of AI.
Empowering Healthcare Providers: Tools and Training for Enhanced Patient Care
To equip healthcare professionals with the necessary skills to leverage AI, organizations must prioritize thorough training programs tailored to various roles within the practice. These programs should encompass not only the technical aspects of using AI tools, but also the ethical considerations and implications for patient care. By integrating real-world scenarios and case studies, providers can gain a deeper understanding of how AI can complement their clinical judgement. Mentorship opportunities pairing experienced staff with those new to technology can also enhance learning pathways, fostering a collaborative surroundings that encourages dialogue around best practices in patient care.
Moreover, deploying user-pleasant platforms that facilitate seamless interaction between healthcare providers and AI tools is critical for prosperous integration. Investing in intuitive interfaces markedly reduces the learning curve associated with new technologies. Creating a support network, including IT personnel and AI specialists, ensures that healthcare workers have continual access to assistance whenever challenges arise.The establishment of feedback loops allows providers to share experiences and improvements, thereby refining AI applications to meet their specific needs. Such an approach not only empowers healthcare providers but also enhances the overall quality of patient care delivered in various settings.